Saving the Osteopathic Profession
The osteopathic profession, which represents the medical degree of doctor of osteopathic medicine, DO, was founded in 1892 by Dr. Andrew Taylor (A.T.) Still. Dr. Still was an allopathic physician, aka MD, during the 1800s. During this time period he lost numerous members of his family to illness, when the conventional practice of medicine was not able to help them. He thought to himself “there has got to be a better way to take care of the patient.” He had the revelation that “health is the normal state in a normal body; disease is the normal state in an abnormal body.”
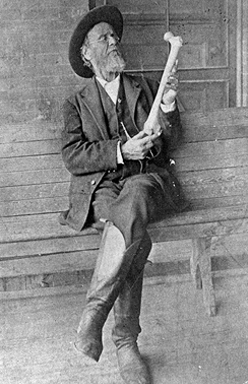
With this in mind, Dr. Still learned to approach his patients with a more holistic philosophy, and he trained himself in the art that is now known as Osteopathic Manipulative Treatment, or OMT, or Osteopathic Manipulative Medicine, OMM. He created a new degree in medicine, to be separate but equal to the conventional allopathic medicine degree of M.D. This degree was the Doctor of Osteopathic Medicine, D.O., and Dr. Still was the first to carry this title (A.T. Still, D.O., M.D.).
The definition of osteopathic medicine is: A complete system of medical care with a philosophy that combines the needs of the patient with the current practice of medicine, surgery and obstetrics; that emphasizes the interrelationship between structure and function; and that has an appreciation of the body’s ability to heal itself.
The osteopathic philosophy is founded on these four principles:
I. The body is a unit; the person is a unit of body, mind, and spirit
II. The body is capable of self-regulation, self-healing, and health maintenance
III. Structure and function are reciprocally interrelated
IV. Rational treatment is based upon an understanding of the basic principles of body unity, self-regulation, and the interrelationship of structure and function
At its inception, the Osteopathic profession struggled for years to gain national (and international) recognition as a legitimate field of medicine. Seemingly every time the osteopathic profession appeared to have its back against the wall, with threats to its distinctive identity and existence, the osteopathic profession has prevailed and persevered. Through many political efforts of osteopathic leadership the osteopathic profession has been widely regarded as equal to the allopathic profession, and DOs and MDs practice side-by-side in all aspects of medicine and surgery since the 1980s.
 While OMM does not define the osteopathic profession, it certainly has provided distinction from our allopathic colleagues. It often reverts to the philosophy of what defines an osteopathic physician, practicing with the aforementioned principles, using that approach for all patient care, and this is something I consistently use in the way I see my patients. It’s the reason I can see someone who has seen numerous other physicians, and I am able to figure out what is going on with them, and what I can do to get them better, when others have not been able to. Using this philosophy allows me a unique way to really get to know what is going on with my patient, who my patient is, and what I need to do to get my patients on a proper path towards wellness.
While OMM does not define the osteopathic profession, it certainly has provided distinction from our allopathic colleagues. It often reverts to the philosophy of what defines an osteopathic physician, practicing with the aforementioned principles, using that approach for all patient care, and this is something I consistently use in the way I see my patients. It’s the reason I can see someone who has seen numerous other physicians, and I am able to figure out what is going on with them, and what I can do to get them better, when others have not been able to. Using this philosophy allows me a unique way to really get to know what is going on with my patient, who my patient is, and what I need to do to get my patients on a proper path towards wellness.
I have several outstanding osteopathic and allopathic colleagues, in numerous different specialty fields; all who do not utilize OMM, but definitely practice with the before-mentioned philosophy. Because of this, they are exemplary in their fields, and patients flock to come and see them. That said, these osteopathic philosophies are not necessarily unique to osteopathic medicine, and allopathic physicians or other healthcare providers can definitely use and adopt these principles to approach their patients. The whole premise of osteopathic medicine is these principles are taught, tested, and reinforced in the education of each osteopathic medical student, so they are more likely to utilize these in future patient care.
One of the current threats osteopathic medicine faces is the amalgamation with the allopathic profession. For years the American Osteopathic Association (AOA) and the Accreditation Council of Graduate Medical Education (ACGME) have had two different pathways for medical students to match into their respective specialty. Allopathic physicians have always completed an ACGME residency, and for years osteopathic physicians have had the option of either going through an AOA accredited residency program, or an ACGME accredited residency program.
In 2014 the AOA and ACGME agreed upon a unified pathway into a single accreditation system. This system allowed greater access of osteopathic graduates to the diversity of different residency programs, and it also opened the door for allopathic medicine graduates to train in osteopathic accredited programs. While this inclusion and equality is definitely a great thing, it has led to further blending of the osteopathic profession with the allopathic profession. If DOs train in MD programs, and MDs train in DO programs, then where is the distinction between the two degrees? That further brings up the question, are two different degrees really needed?
In my humble opinion, I absolutely believe these two degrees deserve to coexist, and I do not want to see the osteopathic profession become amalgamated within the allopathic profession. So, how do we stay distinct? Allopathic medical schools are now starting to pick up on osteopathic principles, and we have MD physicians training in DO programs; so how are they coming out of these programs differently than if they trained in an allopathic residency program?
Many could argue that there is not much that distinguish the two, so it comes back to OMM, we need more DOs who practice OMM. We need this in order to help keep ourselves distinguished, in order to make sure this art, this skill, and this medical degree is not lost in the amalgamation of the professions.
Traditionally osteopathic medicine has attracted those interested in going into primary care, and amongst those, many of these primary care docs used to perform OMM routinely in their practice. Over the more recent years we still continue to see a trend of osteopathic medical students mainly going into primary care fields, but we are seeing less and less of a percentage of these doctors actually using OMM in their practice. So why is this?
I personally do a large amount of OMM in my sports medicine practice, it is the most common procedure I perform. Part of this is because OMM is one of the key factors that drew me towards going to an osteopathic medical school. I practiced on my peers, my wife and my family members as I learned it. My second year of medical school I was a teaching assistant for the OMM class, and then I completed a Pre-Doctoral Fellowship in OMM as well as earned a Masters of Science in Clinical Research & Education in OMM prior to going into residency. In my residency I went to an AOA accredited program in Family Medicine & OMM, where OMT was not just allowed, but it was encouraged, it was precepted, and osteopathic principles and practice were part of every single precepting encounter. After residency I did an osteopathic sports medicine fellowship where again, I was able to routinely use and refine my OMM skills. Since graduating I have remained engaged in OMM education, teaching full-time in the OMM class at the Texas College of Osteopathic Medicine for 5 years and now teaching part-time and precepting students and residents in OMM on my sports medicine rotation.

Has all of this extra training been worth it? Absolutely! I have been able to see, diagnose, and treat conditions on patients that other physicians who don’t routinely perform OMM nor perform the osteopathic structural exam were not able to make the appropriate diagnose, nor provide the appropriate treatment. I’ve been able to get patients better by using OMM purely with the use of my hands. By employing OMM in my practice I am able to save our healthcare system expenses by decreasing the time it takes to get over various injuries and ailments. Because of using OMM I often decrease the need for prescription medications including a decrease in the use of opiates for pain control (which is huge with the current opiate crisis we face) and decrease the need for additional testing because of protracted recoveries; the list goes on and on as to the advantages of being a DO who performs osteopathic manipulation. Further, I have found that working with high-level athletes, notably Olympians, gives me a distinct advantage of being a DO who performs OMM. I am able to offer these athletes a hands-on treatment to help with any injuries or pain, as well as ensure their body is in proper form to optimize their athletic performance. Many of these athletes do not even want to take a Tylenol in fear of potentially failing a drug test and ending their dream of winning Olympic gold, so offering OMM has allowed me to stand out as a physician who can offer more than a pill for pain.
While doing my Masters degree, my thesis was entitled: “Attitudes, Knowledge, and Use of Osteopathic Manipulative Treatment by Osteopathic Sports Medicine Physicians: Is OMT Being Used in the Sports Arena?“ While performing this research I did extensive studies on not just OMM, but into medical education and factors that affect how physicians will typically practice. In the many papers I reviewed, the common factor I found was that post-graduate training, residency, was more effective and influential in establishing the practice habits that a physician is going to have. This was more-so than their medical education, pre-doctoral fellowships, postdoctoral fellowships, as well as influences within their first five years of practice.
So, what is my answer as part of the solution to save the osteopathic medical profession? We need to have more consistent training and reinforcement of OMM in residency programs. At the same time, we also have to have more students who are learning practical OMM during medical school, who will then go into these residencies.
In regard to undergraduate OMM curriculums, currently these curriculums have been cut, class sizes have increased, leading to a decreased amount of hands-on practical experience time in the OMM lab under faculty supervision. This has definitely affected the behaviors of osteopathic medical students and their utilization of OMM. Other factors I feel are certain emphases and de-emphases within the curriculum. Topics such as cranial and visceral osteopathy, are now routinely taught as part of the second year OMM curriculums. While I definitely feel that there is value towards cranial and visceral treatments, I feel these could be learned in a residency setting, and the time spent teaching this could easily be spent learning and reviewing other more practical OMM treatments that could be performed by the primary care physician. There are a minority of medical students who have a more significant affluence towards OMM, and they will be able to have the opportunities to learn these nuanced subcategories of osteopathic manipulation in extra-curricular study groups and in more advanced training. In a limited and contracted two years of hands-on osteopathic education (before going onto their clinical rotations), we need to maximize their time for the students’ benefit. We need to have our curriculums appeal to the majority, not to the minority.
I am for the AOA, as well as the American Academy of Osteopathy (AAO), which governs the OMM components of our training, to take hard look at what is happening to our profession, and how we can save it. If our profession keeps its head down and keeps barreling forward, then by the time we look up we will no longer have a distinct profession to be affiliated with. I truly hope my words here can be found as constructive, and not seen as derogatory toward our current educational model. At the same time, I want our osteopathic leaders to look at our educational model and see if the end-product of doctors graduating from their medical schools and residencies are truly embodying the osteopathic physician they were hoping they would become.
I am extremely proud of my Doctor of Osteopathic Medicine degree. It is a degree that carries with it historical, as well as clinical, significance. I want to see this degree maintained and for our osteopathic profession to continue to flourish!
Comments (7)
I learned from the best!
Well written well said.
Very well thought out essay! I am a Director of Osteopathic Education at a family medicine residency. We are osteopathically recognized and we strive to teach and train osteopathic practice and principles (OPP) to both our MD and DO residents. While I too have mixed feelings on the amalgamation of residencies under the ACGME, it was inevitable for a number of reasons. Having said that, I feel OPP has been subtly influencing the practice of medicine in our country for decades and now we have just put the capstone on the process. The challenge now is to infuse the full wisdom of osteopathic thought into the mainstream practice of medicine in the US. OPP, OMM and OMT are not just for musculoskeletal symptoms, but a thought and practice that recognizes that we are kinetic beings and well as chemical beings. As such our health can be optimized kinetically as well. How we change to that paradigm is the real challenge of this new age of medicine in the US.
PREACH!
It’s good to know that osteopathic professions are equal to the allopathic profession. Maybe there is an osteopathic care near me. If I can find one, that would help because it is just like allopathic.
Just look for a physician with “D.O.” after their name.






This is an excellent (and very much needed) commentary on the future of osteopathic medicine! I too, am proud to be an osteopathic physician and I use OMM daily in my practice (and at home). We have to keep teaching the principles AND the practical application of it in our schools and residency programs!